
Impact of tooth extraction
August 28, 2020
Dens Evagination
September 2, 2020Wisdom Tooth Surgery
Prepared by Dr. Lim Ming Chau, Union Dental Bayan Baru.Impacted tooth is a tooth that is completely or partially unerupted and is blocked from other tooth, bone or soft tissue so that its eruption is unlikely.
The gradual evolutionary reduction of human jaws has resulted in jaws are too small to accommodate their teeth. The third molar (wisdom tooth) is the last tooth to erupt and so it may likely become either impacted or displaced if there is inadequate space for it within the dental arch.
Thus impacted third molars are frequently encountered in routine dental practice and one of the most commonly performed oral surgical procedures.
Many factors govern the decision to advise the removal of an impacted third molar especially the lower third molar. Here are some reasons that indicate one for surgically removal of the impacted third molar.

Pericoronitis
Pericoronitis is inflammation of the soft tissues surrounding the crown of a partially erupted tooth. Recurrent pericoronitis is the commonest indication for the surgically removal of impacted lower third molar.
Dental caries
Food may easily get trapped between the impacted third molar and the second molar and one may find it difficult to keep it clean. The resulting retention of food debris and plaque may cause dental caries involving either the occlusal surface of the third molar or the distal surface of the second molar or in both teeth.
Periodontal disease
The third molar being situated so far behind in the mouth, one may find impossible to keep clean. High incidence of periodontal pocketing distal to the second molar has been observed among those with impacted third molar.
Traumatised soft tissue
Trauma to opposing gums, cheeks, tongue If a third molar erupts out of the normal alignment of teeth, it may cause trauma to the opposing gums, cheeks or tongue.Treatment Procedures & Result

The radiograph image shown normal erupted lower left third molar, and impacted lower right third molar.
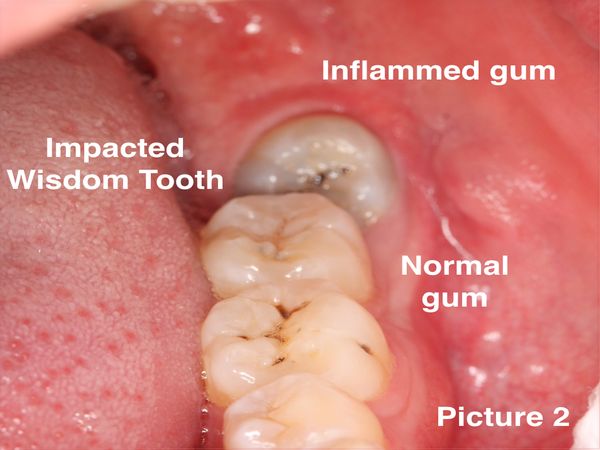
The surrounding gum of impacted third molar was inflamed, swollen and pain, known as Pericoronitis
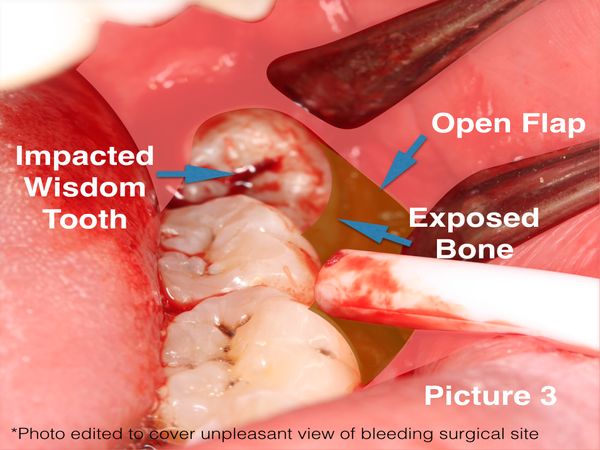
At this stage, surgical removal of impacted lower third molar (wisdom tooth) is necessary. After giving local anaesthesia to numb the surgical area, the gum was carefully cut open to expose the underlying bone and the impacted tooth.

A surgical drill will be used to gutta the bone around the impacted tooth. The impacted wisdom tooth was then cut & divided into several pieces to relief the impaction.
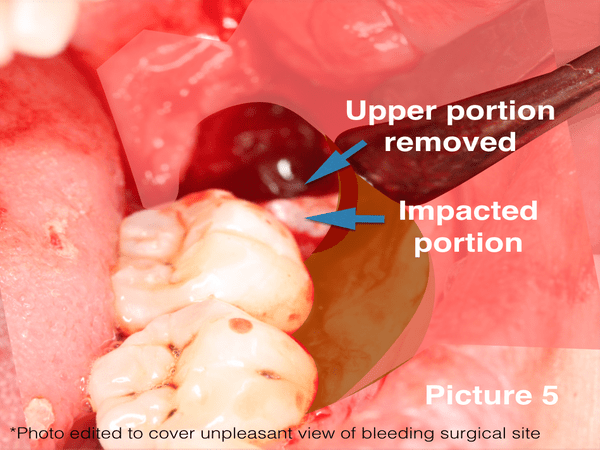
After the tooth being cut into smaller pieces, the fragments was removed piece by piece.

Sometime the fragments of the separated tooth may still having difficulty to remove due to curve root or engaged under the bony undercut. In this situation, we need to do more grinding of that portion to reduce its size, to facilitate removal of all tooth fragments.

After the removal of wisdom tooth, we will attempt to achieve haemostatic (stop bleeding) by applying some direct pressure to help the blood to clot. The soft tissue flap will be stitched (suture) to immobilise it and help to stabilise the blood clot.
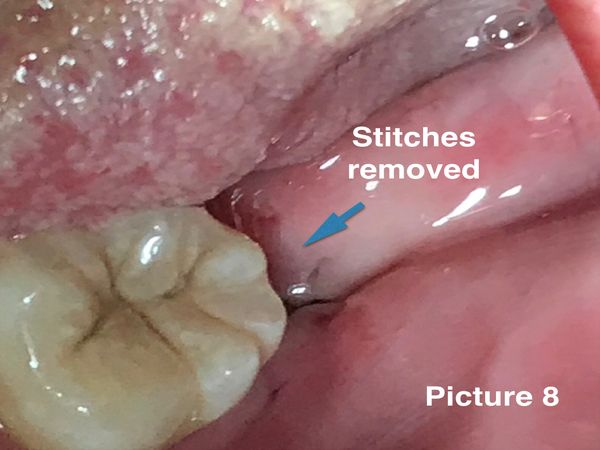
The discomfort and pain may last 2 to 3 days after surgery, but it could be reduced by taking pain killer. Removal of stitches after 10-14days. Soft tissue usually healed within 2 weeks . The whole process of bone remodelling and the tooth socket filled with bone will take 2 months.
Risk & Complications
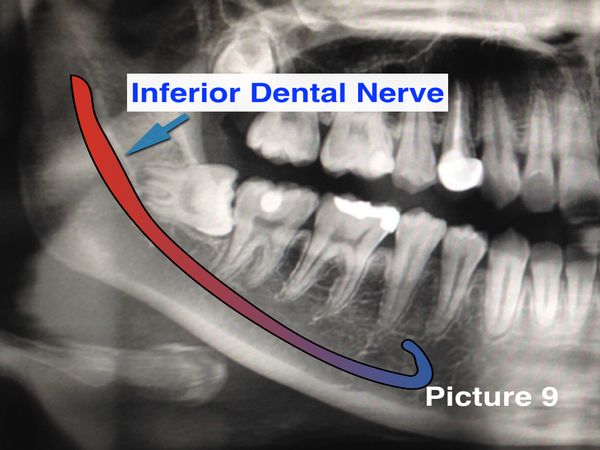
The main concern of complication of wisdom tooth surgery is the injury to the Inferior Dental Nerve (ID), a sensory nerve supply to the cheek, chin & lip. It is a standard procedure to take a radiograph of the impacted wisdom tooth to evaluate the degree of impaction, the extend of decay, the distance from ID Nerve. Then the surgeon will based on the finding to plan the surgery, how wide to open up the gum to expose the impacted wisdom tooth, the depth of surrounding bone to cut away, the safety distance to cut from ID nerve, the direction of cut & divide the wisdom tooth into pieces etc.
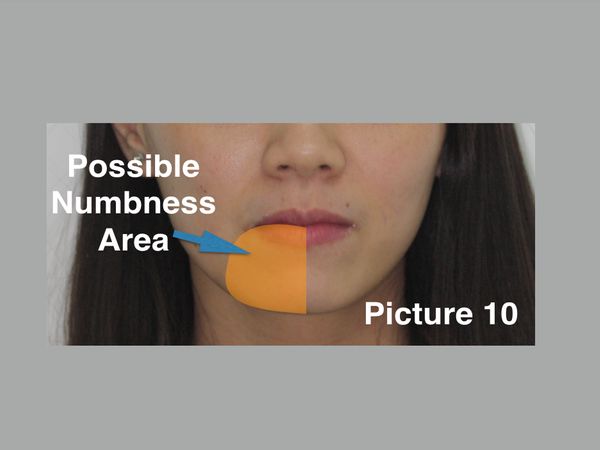
Injury to the ID nerve may cause numbness sensation over it coverage area. Usually the numbness sensation is temporary due to compression of the ID nerve. It will recover gradually within 6-12 months. Prolonged numbness (Paralysis) due to severe nerve injury although might happened, but the chances are low if the treatment procedure are planned properly.
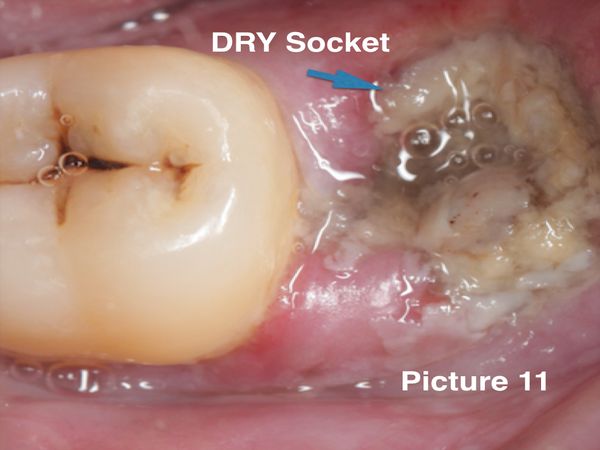
Other possible complications will be prolonged pain & discomfort, usually due to dense socket bone around the wisdom tooth that restrain the blood clot formation, a term known as Dry Socket.
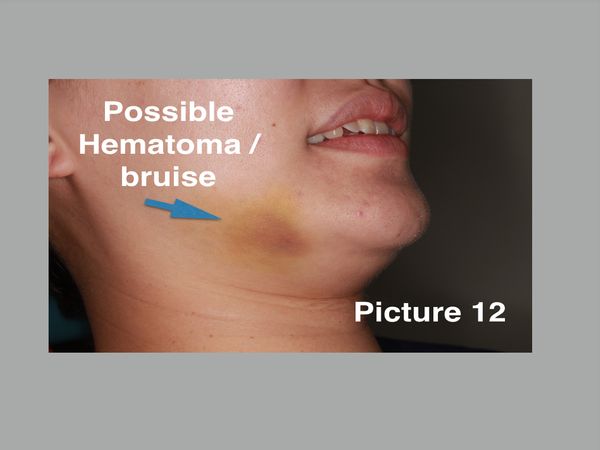
post-operative swelling due to edema (a condition characterised by an excess of watery fluid collecting in the soft tissue) or hematoma (a solid swelling of clotted blood within the tissue), or sometime bruises.



